Treatment of Torus Palatinus: An Overview
Abstract
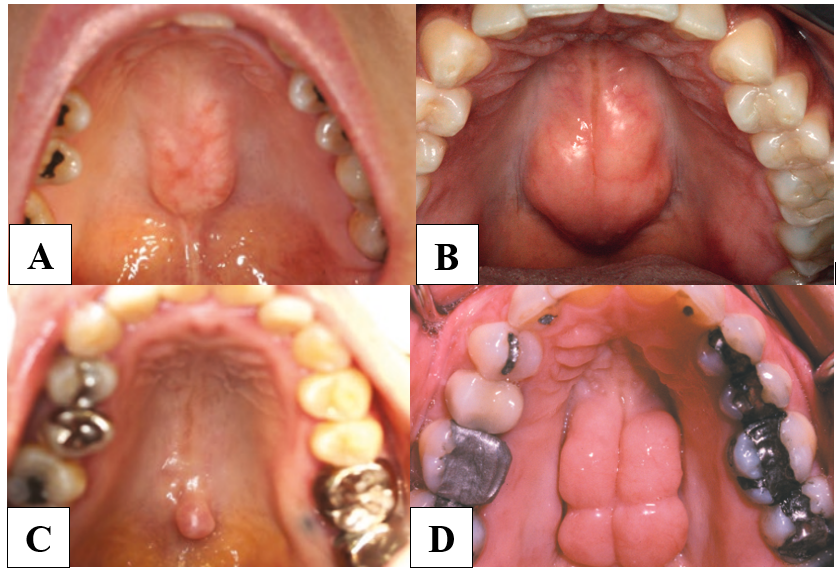
Torus is a non-pathologic exostosis that develops from a localized cortical bone protrusion in the oral cavity. The prevalence of torus palatinus varies from 9% to 60% with predilection for females, with multifactorial etiology. Torus removal or torectomy procedures aim to restore orofacial physiologic function and/or allow placement of rehabilitative prosthetics without risk of harm. Surgical methods for torus removal include traditional methods that use burs, bone chisels, and mallets to remove the bone protrusion; laser surgery, particularly with erbium-doped yttrium aluminum garnet (Er:YAG) lasers, which are less invasive; and piezoelectric surgery, which uses ultrasonic vibrations to cut bone with high precision while protecting soft tissue and causing the least amount of damage to surrounding tissue.
Keywords:
- Torus Palatinus
- Torus Removal
- Palatal exostoses
- Laser ER:YAG
- Piezoelctric
References
Z. Li, Roslan, A. Rahman, and Kamaruddin, “Torus Palatinus and Torus Mandibularis: A Literature Review Update,” Journal of Health and Transational Medicine (JUMMEC), vol. 1, pp. 247–254, 2023.
L. J. Peterson and T. Hupp, Peterson’s Principles of Oral and Maxillofacial Surgery. Cham: Springer International Publishing, 2022. doi: 10.1007/978-3-030-91920-7.
C. L. Gregson et al., “A Rare Mutation in SMAD9 Associated With High Bone Mass Identifies the SMAD-Dependent BMP Signaling Pathway as a Potential Anabolic Target for Osteoporosis,” Journal of Bone and Mineral Research, vol. 35, no. 1, pp. 92–105, Dec. 2020, doi: 10.1002/jbmr.3875.
J. Bouchet, G. Hervé, G. Lescaille, V. Descroix, and A. Guyon, “Palatal torus: etiology, clinical aspect, and therapeutic strategy,” Journal of Oral Medicine and Oral Surgery, vol. 25, no. 2, p. 18, Apr. 2019, doi: 10.1051/mbcb/2018040.
B. W. Neville, C. M. Allen, D. D. Damm, and A. C. Chi, Oral and Maxillofacial Pathology, 4th ed. Missouri: Elsevier, 2016.
J. Iwanaga and R. S. Tubbs, Eds., Anatomical Variations in Clinical Dentistry. Cham: Springer International Publishing, 2019. doi: 10.1007/978-3-319-97961-8.
S. F. Malamed, Handbook of Local Anesthesia, 7th ed. Missouri: Elsevier, 2020.
Ocran E. Palate [Internet], https://www.kenhub.com/en/library/anatomy/the-palate, Kenhub. 2023.
F. D. Fragiskos, Oral Surgery. Berlin: Springer, 2007.
N. A. Malik, Textbook of Oral and Maxillofacial Surgery, Fourth. New Delhi: Jaypee Brothers Medical Publishers, 2016.
J. P. Rocca, H. Raybaud, E. Merigo, P. Vescovi, and C. Fornaini, “Er:YAG Laser: A New Technical Approach to Remove Torus Palatinus and Torus Mandibularis,” Case Rep Dent, vol. 2012, pp. 1–4, 2012, doi: 10.1155/2012/487802.
K. Shibahara, “The Usefulness of Piezoelectric Device in Microscopic Oral Surgery,” Int J Microdent, vol. I, pp. 36–44, 2024.
P. E, G. J, C. E, F. E, and M. A, “Piezosurgery Removal of Mandibular Tori: A Case Series,” Arch Clin Med Case Rep, vol. 07, no. 03, 2023, doi: 10.26502/acmcr.96550615.
R. Dean, B. Ahmed, and H. Sapa, “Surgical removal of torus palatinus in a patient with a history of bisphosphonates,” Faculty Dental Journal, vol. 13, no. 2, pp. 56–61, Apr. 2022, doi: 10.1308/rcsfdj.2022.14.
H. Papadopoulos and T. Lawhorn, “Use of a Palatal Flap for Torus Reduction,” Journal of Oral and Maxillofacial Surgery, vol. 66, no. 9, pp. 1969–1970, Sep. 2008, doi: 10.1016/j.joms.2007.07.007.
-
Article Viewed: 0
Total Download
##plugins.themes.ojsPlusA.frontend.article.downloadstatastics##