The Correlation Study Between Testosterone Levels and Hba1c In Type 2 Diabetic Patients Compare with Healthy Persons
Abstract
The purpose of this study was to evaluate the the connection between hemoglobin glycated (Hba1c) and testosterone levels in the patients of type 2 diabetes mellitus compare with healthy person, also determine the significant differences between this parameter among healthy and diabetic patients, after assumed whole blood and serum specimens from laboratory of Diabetes and Endocrinology Center in Marjan hospital and privately owned in Babylon City starting in October 2022 to February 2023.
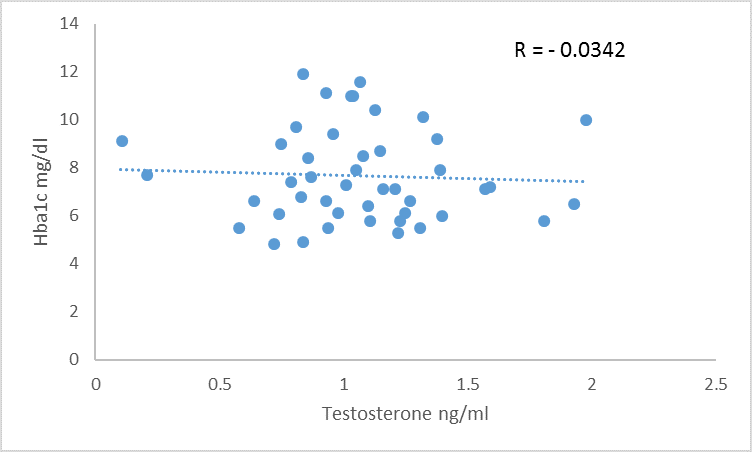
The outcomes showed non-significant (P>0.05) variations between those with diabetes and control groups in age , which refer to all persons in the same age, also it revealed significant increase (P ˂ 0.05) in Hba1c level in diabetic group compare with healthy men, which may refer to disease effect on these patients and lead to elevation in Hba1c in diabetic group, also it was revealed significant decrease (P ˂ 0.05) in diabetic group compare with control in Testosterone level, in addition to significant increase (P˂0.05) in body mass index in diabetic men compare to control group, and The results showed negative correlation between glycated hemoglobin and testosterone levels in both healthy and diabetic men.
The research was concluded that HbA1c value is associated with testosterone levels in diabetic patients.
Keywords:
- Testosterone, Type 2 Diabetic Patients and fertility
References
-Corathers, S., Williford, D.N., Kichler, J. et al. Correction: Implementation of Psychosocial Screening into Diabetes Clinics: Experience from the Type 1 Diabetes Exchange Quality Improvement Network. Curr Diab Rep 23, 29 (2023). https://doi.org/10.1007/s11892-023-01500-8
Zhang, L., Zhang, L., Li, S., Zhang, Q., Luo, Y., Zhang, C., ... & Zhang, C. (2021). Overexpression of mm9_circ_013935 alleviates renal inflammation and fibrosis in diabetic nephropathy via the miR-153-3p/NFIC axis. Canadian journal of physiology and pharmacology,99(11), 1199-1206.
Cole, J. B., & Florez, J. C. (2020). Genetics of diabetes mellitus and diabetes complications. Nature reviews nephrology, 16(7), 377-390.
World Health Organization. (2016). Global report on diabetes: executive summary (No. WHO/NMH/NVI/16.3). World Health Organization.
Kaiafa, G., Veneti, S., Polychronopoulos, G., Pilalas, D., Daios, S., Kanellos, I., ... & Savopoulos, C. (2021). Is HbA1c an ideal biomarker of well-controlled diabetes?. Postgraduate Medical Journal, 97(1148), 380-383.
Chen, J., Yin, D., & Dou, K. (2023). Intensified glycemic control by HbA1c for patients with coronary heart disease and Type 2 diabetes: a review of findings and conclusions. Cardiovascular Diabetology, 22(1), 1-16.
Khera, M., Crawford, D., Morales, A., Salonia, A., & Morgentaler, A. (2014). A new era of testosterone and prostate cancer: from physiology to clinical implications. European urology, 65(1), 115-123.
Adamczewska, D., Słowikowska-Hilczer, J., & Walczak-Jędrzejowska, R. (2022). The fate of leydig cells in men with spermatogenic failure. Life, 12(4), 570.
Nuttall, F. Q. (2015). Body mass index: obesity, BMI, and health: a critical review. Nutrition today, 50(3), 117.
George, A.; Darren, G.; Mallery, D. and Paul, C. (2003). SPSS for windows step by step. Boston, Pearson Education. Inc.pp:55-56.
Eyth, E., & Naik, R. (2019). Hemoglobin A1c.
Joseph, J. J., Deedwania, P., Acharya, T., Aguilar, D., Bhatt, D. L., Chyun, D. A., ... & American Heart Association Diabetes Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Clinical Cardiology; and Council on Hypertension. (2022). Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation, 145(9), e722-e759.
Mahdi, K. S., & AL-Hady, F. A. (2021). Effect of Repaglinide and Metformin As Anti-Diabetic Drugs on Epidydimal Sperm Parameters. Annals of the Romanian Society for Cell Biology, 25(6), 11864-11887.
Wang, Y., & Wang, Y. (2022). Accelerated ovarian aging among type 2 diabetes patients and its association with adverse lipid profile. Frontiers in Endocrinology, 13, 780979.
Kumari, N., Khan, A., Shaikh, U., Lobes, K., Kumar, D., Suman, F. N. U., ... & SUMAN, F. (2021). Comparison of testosterone levels in patients with and without type 2 diabetes. Cureus, 13(7).
Yao, Q. M., Wang, B., An, X. F., Zhang, J. A., & Ding, L. (2018). Testosterone level and risk of type 2 diabetes in men: a systematic review and meta-analysis. Endocrine Connections, 7(1), 220-231.
Oduwole, O. O., Huhtaniemi, I. T., & Misrahi, M. (2021). The roles of luteinizing hormone, follicle-stimulating hormone and testosterone in spermatogenesis and folliculogenesis revisited. International journal of molecular sciences, 22(23), 12735.
Ruze, R., Liu, T., Zou, X., Song, J., Chen, Y., Xu, R., ... & Xu, Q. (2023). Obesity and type 2 diabetes mellitus: connections in epidemiology, pathogenesis, and treatments. Frontiers in Endocrinology, 14, 1161521.
Cai, T., Hu, Y., Ding, B., Yan, R., Liu, B., Cai, L., ... & Ma, J. (2021). Effect of metformin on testosterone levels in male patients with type 2 diabetes mellitus treated with insulin. Frontiers in Endocrinology, 12, 813067.
Simons, P. I., Valkenburg, O., van de Waarenburg, M. P., van Greevenbroek, M. M., Kooi, M. E., Jansen, J. F., ... & Brouwers, M. C. (2023). Serum sex hormone-binding globulin is a mediator of the association between intrahepatic lipid content and type 2 diabetes: the Maastricht Study. Diabetologia, 66(1), 213-222.
Gianatti, E. J., Dupuis, P., Hoermann, R., Strauss, B. J., Wentworth, J. M., Zajac, J. D., & Grossmann, M. (2014). Effect of testosterone treatment on glucose metabolism in men with type 2 diabetes: a randomized controlled trial. Diabetes care, 37(8), 2098-2107.
Farooq, R., Bhat, M. H., Majid, S., & Mir, M. M. (2020). Association between T2DM and the lowering of testosterone levels among Kashmiri males. Archives of endocrinology and metabolism, 64, 528-532.
Kumari, K., Kumar, R., Memon, A., Kumari, B., Tehrim, M., Kumari, P., ... & Kumar, A. (2023). Treatment with Testosterone Therapy in Type 2 Diabetic Hypogonadal Adult Males: A Systematic Review and Meta-Analysis. Clinics and Practice, 13(2), 454-469.
Zhong, S. R., Yang, H. H., Liao, C. H., Yang, D. H., Tu, S. K., Hung, C. L., & Liao, C. C. (2021). Association between low serum testosterone and the development of metabolic syndrome in elderly Taiwanese men. Diabetes, Metabolic Syndrome and Obesity, 99-106.
-
Article Viewed: 0
Total Download
##plugins.themes.ojsPlusA.frontend.article.downloadstatastics##