Possible Interaction Between Drugs for COVID19 And Cancer Therapy
Abstract
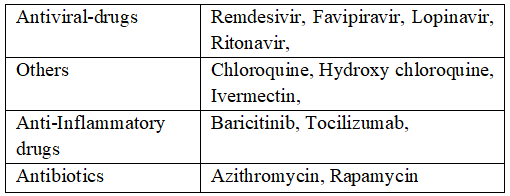
At the end of 2019, a new disease was reported in Wuhan China and described such as severe acute respiratory syndrome (SARS). This new virus named SARSCoV-2 S is characterized by high infectivity among humans. Such disease can have no symptoms in some individuals, while in others can provoke flu like symptoms or acute respiratory distress syndrome, pneumonia, and death. At the end of January 2020, the World Health Organization and Public Health Emergency of International Concern declared a pandemic status. Many studies showed a high mortality rate in cancer patient infected by SARS-CoV-2 infection. In this context, the decision of a safe and effective treatment against COVID19 plays a crucial role crucial in these patients Therefore, important questions arose: Can the COVID19 therapies protect everyone and above all cancer patients? and which drug interactions can occur between cancer therapy and COVID19 treatment? In this regard, Covid-19 is a new disease and for this reason it will be necessary to modify constantly pharmacological treatment. In this scenario, the potential drug–drug interactions (DDI) in the cancer patients should be considered to evaluate the risks and benefits of drug combinations.
Keywords:
- DDI, cancer patients, SARS-CoV2, antineoplastic agents, pharmacological interventions
References
Akbulut M, Urun Y. Onco-cardiology: Drug-drug interactions of antineoplastic and cardiovascular drugs. Crit Rev Oncol Hematol. 145:102822. 2020 doi: 10.1016/j.critrevonc.2019.102822
Alanagreh L, Alzoughool F, Atoum M. (2020). Risk of using hydroxychloroquine as a treatment of COVID-19. Int J Risk Saf Med. 31(3):111-116. doi: 10.3233/JRS-200024.
Albani F, Fusina F, Giovannini A, et al. (2020). Impact of Azithromycin and/or Hydroxychloroquine on Hospital Mortality in COVID-19. J Clin Med. 9(9):2800. doi: 10.3390/jcm9092800
Andreani J., Le Bideau M., Duflot I., et al. (2020). In Vitro Testing of Combined Hydroxychloroquine and Azithromycin on SARS-CoV-2 Shows Synergistic Effect. Microb. Pathog. 145:104228. doi: 10.1016/j.micpath.2020.104228 ]
Al-Tawfiq JA, Al-Homoud AH, Memish ZA. (2020). Remdesivir as a possible therapeutic option for the COVID-19. Travel Med Infect Dis. 34:101615. doi: 10.1016/j.tmaid.2020.101615
Anand K, Ziebuhr J, Wadhwani P, et al., (2003). Coronavirus main proteinase (3CLpro) structure: basis for design of anti-SARS drugs. Science. 300(5626):1763-7.doi: 10.1126/science.1085658
Angus DC, Berry S, Lewis RJ. Et al., (2020). The REMAP-CAP (Randomized Embedded Multifactorial Adaptive Platform for Community-acquired Pneumonia) Study. Rationale and Design. Ann Am Thorac Soc. 17(7):879-891. doi: 10.1513/AnnalsATS.202003-192SD
Aralen (chloroquine) package insert. Bridgewater, NJ: Sanofi-aventis U.S. LLC.; 2018 Oct.
Arbel R, Wolff Sagy Y, Hoshen M, et al. (2022). Nirmatrelvir Use and Severe Covid-19 Outcomes during the Omicron Surge. N Engl J Med. 387(9):790-798. doi: 10.1056/NEJMoa2204919
Arshad S., Kilgore P., Chaudhry Z.S., et al. (2020). Treatment with Hydroxychloroquine, Azithromycin, and Combination in Patients Hospitalized with COVID-19. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 97:396–403. doi: 10.1016/j.ijid.2020.06.099.
Asli R, Abdullah MS, Chong PL,et al. (2020). Case Report: Right Bundle Brunch Block and QTc Prolongation in a Patient with COVID-19 Treated with Hydroxychloroquine. Am J Trop Med Hyg. 103(1):79-82. doi: 10.4269/ajtmh.20-0376.
Ayerbe L, Risco-Risco C, Ayis S. (2020). The Association of Treatment with Hydroxychloroquine and Hospital Mortality in COVID-19 Patients. Intern. Emerg. Med. 15:1501–1506. doi: 10.1007/s11739-020-02505-x
Azanza JR, Mensa J, González Del Castillo J, et al. (2022). Interactions listed in the Paxlovid fact sheet, classified according to risks, pharmacological groups, and consequences. Rev Esp Quimioter. 35(4):357-361. doi: 10.37201/req/054.2022.
Baburaj G, Thomas L, Rao M. (2021). Potential Drug Interactions of Repurposed COVID-19 Drugs with Lung Cancer Pharmacotherapies. Arch Med Res. 52(3):261-269. doi: 10.1016/j.arcmed.2020.11.006
Beigel JH, Tomashek KM, Dodd LE, et al. ACTT-1 Study Group Members. (2020). Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med. 383(19):1813-1826. doi: 10.1056/NEJMoa2007764
Berretta M, Caraglia M, Martellotta F, et al. (2016). Drug-Drug Interactions Based on Pharmacogenetic Profile between Highly Active Antiretroviral Therapy and Antiblastic Chemotherapy in Cancer Patients with HIV Infection. Front Pharmacol. 7:71. doi: 10.3389/fphar.2016.00071
Bosaeed M, Alharbi A, Mahmoud E, et al. (2022). Efficacy of favipiravir in adults with mild COVID-19: a randomized, double-blind, multicentre, placebo-controlled clinical trial. Clin Microbiol Infect. 28(4):602-608. doi: 10.1016/j.cmi.2021.12.026.
Batool S, Vuthaluru K, Hassan A, (2023). Efficacy and Safety of Favipiravir in Treating COVID-19 Patients: A Meta-Analysis of Randomized Control Trials. Cureus.15(1):e33676. doi: 10.7759/cureus.33676
Boffito M (2004). From concept to care: pharmacokinetic boosting of protease inhibitors The PRN Noteb. 2004; 9:15-18 (Published online at www.prn.org: The Published by the Physicians’ Research Network, Inc.®, New York City).
Cai Q, Yang M, Liu D, et al. (2020). Experimental Treatment with Favipiravir for COVID-19: An Open-Label Control Study. Engineering (Beijing). 6(10):1192-1198. doi: 10.1016/j.eng.2020.03.007.
Caly L, Druce JD, Catton MG, et al. (2020). The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antivir Res. 178:104787. doi: 10.1016/j.antiviral.2020.104787
Cao B, Wang Y, Wen D, et al. (2020). A trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 382(19):1787-1799. doi: 10.1056/NEJMoa2001282
Cavalcanti AB, Zampieri FG, Rosa RG, et al. Coalition Covid-19 Brazil I Investigators. (2020). Hydroxychloroquine with or without Azithromycin in Mild-to-Moderate Covid-19. N Engl J Med. 383(21):2041-2052. doi: 10.1056/NEJMoa2019014.
Cellina M, Orsi M, Bombaci F, et al. (2020). Favorable changes of CT findings in a patient with COVID-19 pneumonia after treatment with tocilizumab. Diagn Interv Imaging. 101(5):323-324. doi: 10.1016/j.diii.2020.03.010.
Chan JF, Yao Y, Yeung ML, et al. (2015) Treatment with lopinavir/ritonavir or interferon-β1b improves outcome of MERS-CoV infection in a nonhuman primate model of common marmoset. J Infect Dis. 15;212(12):1904-13.doi:10.1093/infdis/jiv392.
Chary MA, Barbuto AF, Izadmehr S, et al. (2023). COVID-19 Therapeutics: Use, Mechanism of Action, and Toxicity (Xenobiotics). J Med Toxicol. 19(1):26-36. doi: 10.1007/s13181-022-00918-y
Chen F, Chan KH, Jiang Yet al. (2004). In vitro susceptibility of 10 clinical isolates of SARS coronavirus to selected antiviral compounds. J Clin Virol. 31:69–75; 7. doi: 10.1016/j.jcv.2004.03.003.
Chen C, Zhang Y, Huang J, et al. (2021). Favipiravir Versus Arbidol for Clinical Recovery Rate in Moderate and Severe Adult COVID-19 Patients: A Prospective, Multicenter, Open-Label, Randomized Controlled Clinical Trial. Front Pharmacol. 12:683296. doi: 10.3389/fphar.2021.683296
Chen X, Zhao B, Qu Y, et al. (2019). Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated With Drastically Elevated Interleukin 6 Level in Critically Ill Patients With Coronavirus Disease Clin Infect Dis. 71(8):1937-1942. 2020. doi: 10.1093/cid/ciaa449.
Choy KT, Wong AY, Kaewpreedee P, (2020). Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro. Antiviral Res.178:104786. doi: 10.1016/j.antiviral.2020.104786
Chu DJ, Yao DE, Zhuang YF, et al. (2014). Azithromycin enhances the favorable results of paclitaxel and cisplatin in patients with advanced non-small cell lung cancer. Genet Mol Res. 13(2):2796-805 doi: 10.4238/2014.April.14.8.
Cleveland Clinic. A single-arm, open-label, multicenter phase 2 study to evaluate the efficacy and safety of taletrectinib in patients with advanced or metastatic ROS1 positive NSCLC and other solid tumors. https://my.clevelandclinic.org/clinical-trials/1558-a-single-arm-open-label-multicenter-phase-2-study-to-evaluate-the-efficacy-and-safety-of-taletrectinib-in-patients-with-advanced-or-metastatic-ros1-positive-nsclc-and-other-solid-tumors. Accessed September 2, 2022.
ClinicalTrials.gov (2020) ClinicalTrials.gov: a database of privately and publicly funded clinical studies conducted around the world. https://clinicaltrials.gov/ct2/home. Accessed 19 Oct 2020.
ClinicalTrials.gov. A phase I/II, open-label, multicenter student to assess the safety, tolerability, pharmacokinetics and anti-tumor efficacy of DZD9008 (Sunvozertinib) in patients with advanced non-small cell lung cancer (NSCLC) with EGFR or HER2 mutation. https://clinicaltrials.gov/ct2/show/NCT03974022. Accessed September 2, 2022.
Colson P, Rolain JM, Lagier JCet al. (2020). Chloroquine and hydroxychloroquine as available weapons to fight COVID-19. Int J Antimicrob Agents. 55(4):105932. 2020. doi: 10.1016/j.ijantimicag.2020.105932
Coomes EA, Haghbayan H. (2020). Interleukin-6 in Covid-19: A systematic review and meta-analysis. Rev Med Virol. 30(6):1-9. doi: 10.1002/rmv.
Dabbous HM, Abd-Elsalam S, El-Sayed MH, et al. (2021).. Efficacy of favipiravir in COVID-19 treatment: a multi-center randomized study. Arch Virol. 166(3):949-954. doi: 10.1007/s00705-021-04956-9.
Dabbous HM, El-Sayed MH, El Assal G, et al. (2021). Safety and efficacy of favipiravir versus hydroxychloroquine in management of COVID-19: A randomised controlled trial. Sci Rep. 11(1):7282. doi: 10.1038/s41598-021-85227-
Das RR, Jaiswal N, Dev N, et al. (2020). Efficacy and safety of anti-malarial drugs (chloroquine and hydroxy-chloroquine) in treatment of COVID-19 infection: a systematic review and meta-analysis. Front Med (Lausanne) 7:482. doi: 10.3389/fmed.2020.00482.
DiNicolantonio JJ, Barroso J, McCarty M. (2020). Ivermectin may be a clinically useful anti-inflammatory agent for late-stage COVID-19. Open Heart. 7(2):e001350. doi: 10.1136/openhrt-2020
Demir E, Sütcüoğlu O, Demir B, et al. (2022). A possible interaction between favipiravir and methotrexate: Drug-induced hepatotoxicity in a patient with osteosarcoma. J Oncol Pharm Pract. 28(2):445-448. doi: 10.1177/10781552211031304.
Dirim AB, Demir E, Safak Set al. (2020). Hydroxychloroquine-Associated Hypoglycemia in Hemodialysis Patients With COVID-19. Kidney Int Rep. 5(10):1811-1814.doi: 10.1016/j.ekir.2020.06.039.
Du YX, Chen XP. (2020). Favipiravir: Pharmacokinetics and Concerns About Clinical Trials for 2019-nCoV Infection. Clin Pharmacol Ther. 108(2):242-247. doi: 10.1002/cpt.1844.
Echeverría-Esnal D, Martin-Ontiyuelo C, Navarrete-Rouco ME, et al. (2021). Azithromycin in the treatment of COVID-19: a review. Expert Rev Anti Infect Ther. 19(2):147-163. doi: 10.1080/14787210.2020.1813024
Fekete F, Mangó K, Déri M, wr al. (2021). Impact of genetic and non-genetic factors on hepatic CYP2C9 expression and activity in Hungarian subjects. Sci Rep. 11(1):17081. 2021. doi: 10.1038/s41598-021-96590-3.
Food and Drug Administration IRESSA (gefitinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/206995s003lbl.pdf
Food and Drug Administration TAGRISSO™ (osimertinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/208065s000lbl.pdf
Food and Drug Administration EXKIVITY™ (mobocertinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/215310s000lbl.pdf
Food and Drug Administration TUKYSATM (tucatinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213411s000lbl.pdf
Food and Drug Administration XALKORI® (crizotinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/202570s030lbl.pdf
Food and Drug Administration ROZLYTREK (entrectinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/212725s000lbl.pdf 1
Food and Drug Administration TABRECTATM (capmatinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213591s000lbl.pdf
Food and Drug Administration RETEVMOTM (selpercatinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213246s000lbl.pdf
Food and Drug Administration GAVRETO™ (pralsetinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/214701s000lbl.pdf
Food and Drug Administration COTELLIC (cobimetinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/206192s000lbl.pdf
Food and Drug Administration ZELBORAF® (vemurafenib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/202429s012lbl.pdf
Food and Drug Administration BRAFTOVI™ (encorafenib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/210496lbl.pdf Food and Drug Administration TAFINLAR® (dabrafenib) FDA package insert. https://www.access data.fda.gov/drugsatfda_docs/label/2018/202806s010lbl.pdf
Food and Drug Administration MEKINIST® (trametinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/204114s007lbl.pdf
Food and Drug Administration VITRAKVI® (larotrectinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/211710s004lbl.pdf
Food and Drug Administration CABOMETYX® (cabozantinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/208692s003lbl.pdf
Food and Drug Administration LUMAKRAS™ (sotorasib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/214665s000lbl.pdf
Food and Drug Administration ALUNBRIG® (brigatinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/208772s008lbl.pdf
Food and Drug Administration. LORBRENA® (lorlatinib) FDA package insert. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/210868s004lbl.pdf. Accessed 02 September 2, 2022.
Furuta Y, Takahashi K, Shiraki K, Sakamoto K, Smee DF, Barnard DL, Gowen BB, Julander JG, Morrey JD. T-705 (favipiravir) and related compounds: Novel broad-spectrum inhibitors of RNA viral infections. Antiviral Res. 82(3):95-102. 2009. doi: 10.1016/j.antiviral.2009.02.198.
Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Tissot Dupont H, Honoré S, Colson P, Chabrière E, La Scola B, Rolain JM, Brouqui P, Raoult D. (2020). Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 56(1):105949. doi: 10.1016/j.ijantimicag.2020.
Gay C, Toulet D, Le Corre P. (2017). Pharmacokinetic drug-drug interactions of tyrosine kinase inhibitors: A focus on cytochrome P450, transporters, and acid suppression therapy. Hematol Oncol. 35(3):259-280. doi: 10.1002/hon.2335
Geleris J, Sun Y, Platt J,et al. (2020).. Observational Study of Hydroxychloroquine in Hospitalized Patients with Covid-19. N Engl J Med. 382(25):2411-2418. doi: 10.1056/NEJMoa2012410
Giudicessi JR, Noseworthy PA, Friedman PA, et al. (2020). Urgent Guidance for Navigating and Circumventing the QTc-Prolonging and Torsadogenic Potential of Possible Pharmacotherapies for Coronavirus Disease 19 (COVID-19). Mayo Clin Proc. 95(6):1213-1221.doi: 10.1016/j.mayocp.2020.03.024.
Goldman JD, Lye DCB, Hui DS, et al, GS-US-540-5773 Investigators. (2020). Remdesivir for 5 or 10 days in patients with severe Covid-19. N Engl J Med. 383(19):1827–1837. oi:10.1056/NEJMoa2015301
González Canga A, Sahagún Prieto AM, Diez Liébana MJ, et al. (2008). The pharmacokinetics and interactions of ivermectin in humans--a mini-review. AAPS J. 10(1):42-6. doi: 10.1208/s12248-007-9000-9.
Gordon AC, Mouncey PR, Al-Beidh F, et al. REMAP-CAP Investigators. (2021). Interleukin-6 Receptor Antagonists in Critically Ill Patients with Covid-19. N Engl J Med. 384(16):1491-1502. doi: 10.1056/NEJMoa2100433
Gordon CJ, Tchesnokov EP, Feng JY, et al. (2020). The antiviral compound remdesivir potently inhibits RNA-dependent RNA polymerase from Middle East respiratory syndrome coronavirus. J Biol Chem. 295(15):4773-4779. 2020. doi: 10.1074/jbc.AC120.
Grange S, Schmitt C, Banken L, et al. (2011). Thorough QT/QTc study of tocilizumab after single-dose administration at therapeutic and supratherapeutic doses in healthy subjects. Int J Clin Pharmacol Ther. 49(11):648-55. 2011. doi: 10.5414/cp201549
Grivas P, Khaki AR, Wise-Draper TM, et al. (2021). Association of clinical factors and recent anticancer therapy with COVID-19 severity among patients with cancer: a report from the COVID-19 and Cancer Consortium. Ann Oncol. 32(6):787-800. doi: 10.1016/j.annonc.2021.02.024
Guérin V, Lévy P, Thomas JL, et al. (2020). Azithromycin and Hydroxychloroquine Accelerate Recovery of Outpatients with Mild/Moderate COVID-19. Asian J. Med. Heal. 18:15–55. doi: 10.9734/ajmah/2020/v18i730224
Gyselinck I, Janssens W, Verhamme P, et al. (2021). Rationale for azithromycin in COVID-19: an overview of existing evidence. BMJ Open Respir Res. 8(1):e000806. doi: 10.1136/bmjresp-2020-000806.
Hammond J, Leister-Tebbe H, Gardner A, et al. ; EPIC-HR Investigators. (2022). Oral Nirmatrelvir for High-Risk, nonhospitalized adults with Covid-19. N Engl J Med. 386(15):1397-1408. doi: 10.1056/NEJMoa2118542.
Hashemian SMR, Sheida A, Taghizadieh M, et al. (2023). Paxlovid (Nirmatrelvir/Ritonavir): A new approach to Covid-19 therapy? Biomed Pharmacother. 162:114367. doi: 10.1016/j.biopha.2023.114367
Hassan SN, Mohamed Yusoff AA, et al. (2022). Exploring the cytotoxicity and anticancer effects of doxycycline and azithromycin on human glioblastoma multiforme cells. Neurol Res. 44(3):242-251. doi: 10.1080/01616412.2021.1975225.
Hernandez AV, Roman YM, Pasupuleti V, et al. (2020). Update Alert 2: Hydroxychloroquine or Chloroquine for the Treatment or Prophylaxis of COVID-19. Ann Intern Med. 173(7):W128-W129. doi: 10.7326/L20-1054
Horby P, Lim WS, Emberson JR, et al. (2021). Dexamethasone in Hospitalized Patients with Covid-19. N Engl J Med. 384(8):693-704. doi: 10.1056/NEJMoa2021436.
Huang M, Li M, Xiao F, et al. (2020). Preliminary evidence from a multicenter prospective observational study of the safety and efficacy of chloroquine for the treatment of COVID-19. Natl Sci Rev. 7(9):1428–1436. doi: 10.1093/nsr/nwaa113
Huang M, Tang T, Pang P, et al. (2020). Treating COVID-19 with chloroquine. J Mol Cell Biol. 2020;12(4):322-325. 2020. doi: 10.1093/jmcb/mjaa014
Iketani S, Mohri H, Culbertson B, et al. (2023). Multiple pathways for SARS-CoV-2 resistance to nirmatrelvir. Nature. 613(7944):558-564. doi: 10.1038/s41586-022-05514-2.
Imanova Yaghji N, Kan EK, et al. (2021). Hydroxychloroquine Sulfate Related Hypoglycemia In A Non-Diabetic COVİD-19 Patient: A Case Report and Literature Review. Postgrad Med. 133(5):548-551. doi: 10.1080/00325481.2021.1889820
Islam JY, Vidot DC, Camacho-Rivera M. (2021). Evaluating Mental Health-Related Symptoms Among Cancer Survivors During the COVID-19 Pandemic: An Analysis of the COVID Impact Survey. JCO Oncol Pract. 17(9):e1258-e1269. doi: 10.1200/OP.20.00752
Jans DA, Wagstaff KM. (2020), Ivermectin as a broad-spectrum host-directed anti-viral: the real deal? Cells. 9:2100. doi: 10.3390/cells9092100.
JA OS. EUA 105 Pfizer Paxlovid LOA (12222021). In: Administration USFaD, editor. 2021
Jiang L, Wang P, Sun YJ, et al. (2019). Ivermectin reverses the drug resistance in cancer cells through EGFR/ERK/Akt/NF-κB pathway. J Exp Clin Cancer Res. 38(1):265.doi: 10.1186/s13046-019-1251-7.
Kalil AC, Patterson TF, Mehta AK, et al. ACTT-2 Study Group Members. (2021). Baricitinib plus Remdesivir for Hospitalized Adults with Covid-19. N Engl J Med. 384(9):795-807. doi: 10.1056/NEJMoa2031994
Kamel AM, Monem MSA, Sharaf NA, et al. (2022). Efficacy and Safety of Azithromycin in COVID-19 Patients: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Rev. Med. Virol. 32:e2258. doi: 10.1002/rmv.2258
Kuderer NM, Choueiri TK, Shah DP, et al,COVID-19 and Cancer Consortium (2020). Clinical Impact of COVID-19 on Patients with Cancer (CCC19): A Cohort Study. Lancet (Lond. Engl.) 395:1907–1918. doi: 10.1016/S0140-6736(20)31187-9.
Kumar D, Trivedi N. (2021). Disease-drug and drug drug interaction in COVID-19: risk and assessment. Biomed Pharmacother 139: 111642. doi: 10.1016/j.biopha.2021.111642
Lammers AJJ, Brohet RM, Theunissen REP, et al. (2021). Response to correspondence concerning: "Early hydroxychloroquine but not chloroquine use reduces ICU admission in COVID-19 patients". Int J Infect Dis. 103:478-479. doi: 10.1016/j.ijid.2020.12.008 .
Lee KA, Ma W, Sikavi DR, et al., COPE consortium. Cancer and Risk of COVID-19 (2021). Through a General Community Survey. Oncologist. 26, 182–185. doi: 10.1634/theoncologist.2020-0572
Lehrer A, Rheinstein PH. (2020) Ivermectin docks to the SARS-CoV-2 spike receptor binding domain attached to ACE2. In vivo. 34:3023–3026.2020. doi: 10.21873/invivo.12134.
Li P, Wang Y, Lavrijsen M, et al. (2022). SARS-CoV-2 Omicron variant is highly sensitive to molnupiravir, nirmatrelvir, and the combination. Cell Res. 32(3):322-324. doi: 10.1038/s41422-022-00618-w.
Lamb R, Ozsvari B, Lisanti CL, et al. (2015). Antibiotics that target mitochondria effectively eradicate cancer stem cells, across multiple tumor types: treating cancer like an infectious disease. Oncotarget. 6(7):4569-84. 2015. doi: 10.18632/oncotarget.3174
Lauriola M, Pani A, Ippoliti G, et al. (2020). Effect of Combination Therapy of Hydroxychloroquine and Azithromycin on Mortality in Patients With COVID-19. Clin. Transl. Sci. 13:1071–1076. doi: 10.1111/cts.12860.
Lemaitre F, Grégoire M, Monchaud C, et al. (2022). Therapeutic Drug Monitoring and Treatment Personalization group (STP-PT) of the French Society of Pharmacology and Therapeutics (SFPT); French Pharmacovigilance Network (CRPV); ANRS-MIE AC-43 Clinical Pharmacology Committee, joint working group; SFPT Therapeutic Drug Monitoring and Treatment Personalization group (STP-PT) of the French Society of Pharmacology and Therapeutics (SFPT); French Pharmacovigilance Network (CRPV); ANRS-MIE AC-43 Clinical Pharmacology Committee, joint working group. Management of drug-drug interactions with nirmatrelvir/ritonavir in patients treated for Covid-19: Guidelines from the French Society of Pharmacology and Therapeutics (SFPT). Therapie. 77(5):509-521. doi: 10.1016/j.therap.2022.03.005
Li F, Huang J, Ji D, Meng Q, et al. (2017). Azithromycin effectively inhibits tumor angiogenesis by suppressing vascular endothelial growth factor receptor 2-mediated signaling pathways in lung cancer. Oncol Lett. 14(1):89-96. doi: 10.3892/ol.2017.6103
Liang W, Guan W, Chen R, et al. (2020). Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 21, 335–337. doi: 10.1016/S1470-2045(20)30096-6.
Lou Y, Liu L, Yao H, et al. (2021). Clinical Outcomes and Plasma Concentrations of Baloxavir Marboxil and Favipiravir in COVID-19 Patients: An Exploratory Randomized, Controlled Trial. Eur J Pharm Sci. 157:105631. doi: 10.1016/j.ejps.2020.105631
Lv, Z., Chu Y, Wang Y. (2015). HIV protease inhibitors: a review of molecular selectivity and toxicity. HIV AIDS (Auckl). 7:95-104. doi: 10.2147/HIV.S79956
Makinson A, Pujol JL, Le Moing V, et al. (2010). Interactions between cytotoxic chemotherapy and antiretroviral treatment in human immunodeficiency virus-infected patients with lung cancer. J Thorac Oncol. 5(4):562-71. doi: 10.1097/JTO.0b013e3181d3ccf2.
Malden DE, Hong V, Lewin BJ, et al. (2022). Hospitalization and Emergency Department Encounters for COVID-19 After Paxlovid Treatment - California, December 2021-May 2022. MMWR Morb Mortal Wkly Rep. 71(25):830-833. doi: 10.15585/mmwr.mm7125e2.
McIntyre RS and Lee Y. (2020). Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Research. 294: 113492. doi:10.1016/j.psychres.2020.113104
Mealey KL, Northrup NC, Bentjen SA. (2003). Increased toxicity of P-glycoprotein-substrate chemotherapeutic agents in a dog with the MDR1 deletion mutation associated with ivermectin sensitivity. J Am Vet Med Assoc. 223(10):1453-5, 1434. doi: 10.2460/javma.2003.223.1453. PMID: 14627096
Ménez C, Mselli-Lakhal L, Foucaud-Vignault M, et al. (2012). Ivermectin induces P-glycoprotein expression and function through mRNA stabilization in murine hepatocyte cell line. Biochem Pharmacol. 83(2):269-78. 2012. doi: 10.1016/j.bcp.2011.10.010
Mealey KL, Northrup NC, Bentjen SA. (2003). Increased toxicity of P-glycoprotein-substrate chemotherapeutic agents in a dog with the MDR1 deletion mutation associated with ivermectin sensitivity. J Am Vet Med Assoc. 223(10):1453-5, 1434. doi: 10.2460/javma.2003.223.1453
Mitja O, Clotet B. (2020). Use of antiviral drugs to reduce COVID-19 transmission. Lancet Glob Health 8: e639-e640. doi: 10.1016/S2214-109X(20)30114-5
Mody V, Ho J, Wills S, Mawri A et al. (2021). Identification of 3-chymotrypsin like protease (3CLPro) inhibitors as potential anti-SARS-CoV-2 agents. Commun Biol. 4(1):93. 2021. doi: 10.1038/s42003-020-01577-x
Moriya S, Che X-F, Komatsu S, et al. (2013). Macrolide antibiotics block autophagy flux and sensitize to bortezomib via endoplasmic reticulum stress-mediated CHOP induction in myeloma cells. Int J Oncol. 42(5):1541–1550. doi: 10.3892/ijo.2013.1870.
Mukai S, Moriya S, Hiramoto M, et al. (2016).. Macrolides sensitize EGFR-TKI-induced non-apoptotic cell death via blocking autophagy flux in pancreatic cancer cell lines. Int J Oncol. 48(1):45-54. doi: 10.3892/ijo.2015.
Najjar-Debbiny R, Gronich N, Weber G, et al. (2023). Effectiveness of Paxlovid in Reducing Severe Coronavirus Disease 2019 and Mortality in High-Risk Patients. Clin Infect Dis. 76(3):e342-e349. doi: 10.1093/cid/ciac443
National Institute of Health. The Covid-19 Treatment Guidelines Panel's Statement on the Use of Ivermectin for the Treatment of Covid-19. 2021.
Nicolò M, Ferro Desideri L, Bassetti M, et al. (2021). Hydroxychloroquine and chloroquine retinal safety concerns during COVID-19 outbreak. Int Ophthalmol. 41(2):719-725. .doi: 10.1007/s10792-020-01593-0.
Nunes M, Duarte D, Vale N, et al. (2022).. Pitavastatin and Ivermectin Enhance the Efficacy of Paclitaxel in Chemoresistant High-Grade Serous Carcinoma. Cancers (Basel). 14(18):4357.2022. doi: 10.3390/cancers1418435
Oldfield V, Dhillon S, Plosker GL. (2009). Tocilizumab: a review of its use in the management of rheumatoid arthritis. Drugs. 69(5):609-32. doi: 10.2165/00003495-200969050-00007
Owen DR, Allerton CMN, Anderson AS, et al. (2021). An oral SARS-CoV-2 Mpro inhibitor clinical candidate for the treatment of COVID-19. Science. 374(6575):1586-1593. doi: 10.1126/science.abl4784
Pan H, Peto R, Henao-Restrepo AM et al. (2021). Repurposed Antiviral Drugs for Covid-19 - Interim WHO Solidarity Trial Results. N Engl J Med. 384(6):497-511. doi: 10.1056/NEJMoa2023184.
Peluso MJ, Anglin K, Durstenfeld MS, et al. (2022). Effect of Oral Nirmatrelvir on Long COVID Symptoms: 4 Cases and Rationale for Systematic Studies. Pathog Immun. 7(1):95-103. doi: 10.20411/pai.v7i1.518.
Pharmaceuticals and Medical Devices Agency: Avigan (favipiravir) Review Report 2014 https://www.pmda.go.jp/files/000210319.pdf. (Accessed April 15 2020).
Pillai VC, Parise RA, Christner SM, et al. (2014). Potential interactions between HIV drugs, ritonavir and efavirenz and anticancer drug, nilotinib--a study in primary cultures of human hepatocytes that is applicable to HIV patients with cancer. J Clin Pharmacol. 54(11):1272-9. doi: 10.1002/jcph.333
Popp M, Reis S, Schießer S, et al. (2022). Ivermectin for preventing and treating COVID-19. Cochrane Database Syst Rev. 6(6):CD015017. doi: 10.1002/14651858.CD015017
Qiao X, Wang X, Shang Y, Li Y, et al. (2018).. Azithromycin enhances anticancer activity of TRAIL by inhibiting autophagy and up-regulating the protein levels of DR4/5 in colon cancer cells in vitro and in vivo. Cancer Commun (Lond). 38(1):43.doi: 10.1186/s40880-018-0309-9.
Reis G, Moreira Silva EADS, et al; TOGETHER Investigators. (2021). Effect of Early Treatment with Hydroxychloroquine or Lopinavir and Ritonavir on Risk of Hospitalization Among Patients with COVID-19: The TOGETHER Randomized Clinical Trial. JAMA Netw Open. 4(4):e216468. doi: 10.1001/jamanetworkopen.2021.6468.
Rehman SU, Rehman SU, Yoo HH. (2021). COVID-19 challenges and its therapeutics. Biomed Pharmacother. 142:112015. doi: 10.1016/j.biopha.2021.112015
Rivera DR, Peters S, Panagiotou OA; et al. COVID-19 and Cancer Consortium. (2020). Utilization of COVID-19 treatments and clinical outcomes among patients with cancer: a COVID-19 and cancer consortium (CCC19) cohort study. Cancer Discov.10: 1514–1527.
Rezaee H, Pourkarim F, Pourtaghi-Anvarian S, et al. (2021). Drug-drug interactions with candidate medications used for COVID-19 treatment: An overview. Pharmacol Res Perspect. 9(1):e00705. doi: 10.1002/prp2.705.
Rismanbaf A. (2020). Potential treatments for COVID-19; a narrative literature review. Arch Acad Emerg Med 8: e29.
Roche Pharma, A. RoActemra 20 mg/mL concentrate for solution for infusion. Eu Summary of Product Characteristics 2013
Rosas IO, Bräu N, Waters M, et al. (2021). Tocilizumab in Hospitalized Patients with Severe Covid-19 Pneumonia. N Engl J Med. 384(16):1503-1516. doi: 10.1056/NEJMoa2028700.
Rosenberg ES, Dufort EM, Udo T, et al. (2020). Association of Treatment With Hydroxychloroquine or Azithromycin With In-Hospital Mortality in Patients With COVID-19 in New York State. JAMA. 323(24):2493-2502. . doi: 10.1001/jama.2020.8630.
Rudek MA, Flexner C, Ambinder RF. (2011). Use of antineoplastic agents in patients with cancer who have HIV/AIDS. Lancet Oncol. 12(9):905-12. doi: 10.1016/S1470-2045(11)70056-0
Salama C, Han J, Yau L, et al. (2021). Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N Engl J Med. 384(1):20-30.. doi: 10.1056/NEJMoa2030340
Schmitt C, Kuhn B, Zhang X, et al. (2012). Tocilizumab has no clinically relevant effects on methotrexate pharmacokinetics in patients with rheumatoid arthritis. Int J Clin Pharmacol Ther. 50(3):218-23. doi: 10.5414/cp201613
Schmitt C, Kuhn B, Zhang X, et al. (2011).. Disease-drug-drug interaction involving tocilizumab and simvastatin in patients with rheumatoid arthritis. Clin Pharmacol Ther. 89(5):735-40. doi: 10.1038/clpt.2011.35
Sekhavati E, Jafari F, SeyedAlinaghi S, et al. (2020). Safety and effectiveness of azithromycin in patients with COVID-19: An open-label randomised trial. Int J Antimicrob Agents. 56(4):106143. doi: 10.1016/j.ijantimicag.2020.106143
Shah MM, Joyce B, Plumb ID, et al. (2023). Paxlovid associated with decreased hospitalization rate among adults with COVID-19 - United States, April-September 2022. Am J Transplant. 23(1):150-155. doi: 10.1016/j.ajt.2022.12.004
Sheahan TP, Sims AC, Leist SR, (2020). Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV Comparative therapeutic efficacy of remdesivir and combination lopinavir, ritonavir, and interferon beta against MERS-CoV. Nat Commun. 11(1):222. doi: 10.1038/s41467-019-13940-6.
Sheppard M, Laskou F, Stapleton PP et al. (2017). Tocilizumab (Actemra). Hum Vaccin Immunother. 13(9):1972-1988. doi: 10.1080/21645515.2017.1316909.
Shinkai M, Tsushima K, Tanaka S, et al. (2021).. Efficacy and Safety of Favipiravir in Moderate COVID-19 Pneumonia Patients without Oxygen Therapy: A Randomized, Phase III Clinical Trial. Infect Dis Ther. 10(4):2489-2509. doi: 10.1007/s40121-021-00517.
Sobreira da Silva MJ, Serpa Osorio-de-Castro CG, Paes RD, et al. (2022). Potential interactions between antineoplastic agents and medicines used to treat Covid-19. J Oncol Pharm Pract. 28(8):1737-1748. doi: 10.1177/10781552211040494
Solaymani-Dodaran M, Ghanei M, Bagheri M, et al. (2021). Safety and efficacy of Favipiravir in moderate to severe SARS-CoV-2 pneumonia. Int Immunopharmacol. 95:107522. doi: 10.1016/j.intimp.2021.107522
Somers EC, Eschenauer GA, Troost JP, et al. (2021). Tocilizumab for Treatment of Mechanically Ventilated Patients With COVID-19. Clin Infect Dis. 73(2):e445-e454. doi: 10.1093/cid/ciaa954
Spinner CD, Gottlieb RL, Criner GJ, et al, for the GS-US-540-5774 Investigators. (2020). Effect of Remdesivir vs standard care on clinical status at 11 days in patients with moderate COVID-19: A Randomized Clinical Trial. Jama. 324(11):1048–1057. doi:10.1001/jama.2020.16349.
Sun Y, Niu W, Du F, et al. (2016).. Safety, pharmacokinetics, and antitumor properties of anlotinib, an oral multi-target tyrosine kinase inhibitor, in patients with advanced refractory solid tumors. J Hematol Oncol. 9(1):105. doi: 10.1186/s13045-016-0332-8
Szente Fonseca SN, de Queiroz Sousa A, Wolkoff AG, et al. (2020). Risk of hospitalization for Covid-19 outpatients treated with various drug regimens in Brazil: Comparative analysis. Travel Med Infect Dis. 38:101906. doi: 10.1016/j.tmaid.2020.101906
Tanriverdl E, Çörtük M, Yildirim BZ, et al. (2021). Hydroxychloroquine plus Azithromycin and Early Hospital Admission Are Beneficial in COVID-19 Patients: Turkish Experience with Real-Life Data. Turkish J. Med. Sci. 51:10–15. doi: 10.3906/sag-2005-82.
Tchesnokov EP, Feng JY, Porter DP, et al. (2019). Mechanism of Inhibition of Ebola Virus RNA-Dependent RNA Polymerase by Remdesivir. Viruses. 11(4):326. doi: 10.3390/v11040326
Touret F., Gilles M., Barral K., et al. (2020). In Vitro Screening of a FDA Approved Chemical Library Reveals Potential Inhibitors of SARS-CoV-2 Replication. Sci. Rep. 10:13093. doi 10.1038/s41598-020-70143-6.
Trivedi N, Verma A, Kumar D. (2020). Possible treatment and strategies for COVID-19: review and assessment. Eur Rev Med Pharmacol Sci;24: 12593-12608. doi: 10.26355/eurrev_202012_24057.
Udwadia ZF, Singh P, Barkate H, et al. (2021). Efficacy and safety of favipiravir, an oral RNA-dependent RNA polymerase inhibitor, in mild-to-moderate COVID-19: A randomized, comparative, open-label, multicenter, phase 3 clinical trial. Int J Infect Dis. 103:62-71. doi: 10.1016/j.ijid.2020.11.142
Vangeel L, Chiu W, De Jonghe S, et al. (2022). Remdesivir, Molnupiravir and Nirmatrelvir remain active against SARS-CoV-2 Omicron and other variants of concern. Antiviral Res. 198:105252. doi: 10.1016/j.antiviral.2022.105252
Wadud N, Ahmed N, Shergill M, et al. (2020). Improved survival outcome in patients with sars-cov-2 (covid-19) ards with tocilizumab administration. Chest. 158(4):A696–7. doi: 10.1016/j.chest.2020.08.654.
Wang M, Cao R, Zhang L, et al. (2020). Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 30(3):269-271. doi: 10.1038/s41422-020-0282-0.
Wang Y, Zhang D, Du G, et al. (2020). Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 395(10236):1569-1578. doi: 10.1016/S0140-6736(20)31022-9.
Wilde AH, Jochmans D, Posthuma CC. (2014).Screening of an FDA-approved compound library identifies four small-molecule inhibitors of Middle East respiratory syndrome coronavirus replication in cell culture. Antimicrob Agents Chemother.58:4875–4884. doi: 10.1128/AAC.03011-14.
World Health Organization. Therapeutics and COVID-19: Living Guideline. Geneva, Switzerland: WHO; 2021. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-therapeutics-2021.1. Accessed April 8, 2021.
World Health Organization: WHO coronavirus (COVID-19) dash board. (2022). Accessed: May 13, 2022; https://data.who.int/dashboards/covid19/cases?n=
Wu KC, Lin CJ .(2019). The regulation of drug-metabolizing enzymes and membrane transporters by inflammation: Evidences in inflammatory diseases and age-related disorders. J Food Drug Anal. 27(1):48-59. doi: 10.1016/j.jfda.2018.11.005.
Xu J, Chen C, Sun K, et al. (2023). Tocilizumab (monoclonal anti-IL-6R antibody) reverses anlotinib resistance in osteosarcoma. Front Oncol. 13:1192472. doi: 10.3389/fonc.2023.1192472.
Xu X, Han M, Li T, et al. (2020). Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci U S A. 117(20):10970-10975. doi: 10.1073/pnas.2005615117
Yu B, Li C, Chen P, et al. (2020). Low dose of hydroxychloroquine reduces fatality of critically ill patients with COVID-19. Sci China Life Sci. 63 (10):1515-1521. doi: 10.1007/s11427-020-17
Zhan X, Dowell S, Shen Y, Lee DL. (2020). Chloroquine to fight COVID-19: A consideration of mechanisms and adverse effects? Heliyon. 6(9):e04900. doi: 10.1016/j.heliyon.2020.e04900.
Zhang X, Song K, Tong F, et al. (2020). First case of COVID-19 in a patient with multiple myeloma successfully treated with tocilizumab. Blood Adv. 4(7):1307-1310. doi: 10.1182/bloodadvances.2020001907
Zhang L, Zhu F, Xie L, et al. (2020). Clinical characteristics of COVID-19-infected cancer patients: A retrospective case study in three hospitals within Wuhan, China. Ann. Oncol. 31, 894–90. 2020. doi: 10.1016/j.annonc.2020.03.296.
Zhao H, Zhu Q, Zhang C, et al. (2021). Tocilizumab combined with favipiravir in the treatment of COVID-19: A multicenter trial in a small sample size. Biomed Pharmacother. 133:110825. doi: 10.1016/j.biopha.2020.1108
Zhong CC, Chen F, Yang JL, et al. (2018). Pharmacokinetics and disposition of anlotinib, an oral tyrosine kinase inhibitor, in experimental animal species. Acta Pharmacol Sin. 39(6):1048-1063. doi: 10.1038/aps.2017.199
Zhou P, Yang XL, Wang XG, et al. (2020). A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 579:270–273. doi: 10.1038/s41586-020-2951-z.
Zhou X, Zhang Y, Li Y, Hao X, et al. (2012). Azithromycin synergistically enhances anti-proliferative activity of vincristine in cervical and gastric cancer cells. Cancers. 4(4):1318–1332. doi:10.3390/cancers4041318
Zou HX, Zhang YF, Zhong DF et al. (2022). Effect of autoinduction and food on the pharmacokinetics of furmonertinib and its active metabolite characterized by a population pharmacokinetic model. Acta Pharmacol Sin. 43(7):1865-1874. doi: 10.1038/s41401-021-00798-y.
-
Article Viewed: 0
Total Download
##plugins.themes.ojsPlusA.frontend.article.downloadstatastics##